Postural Orthostatic Tachycardia Syndrome (POTS)
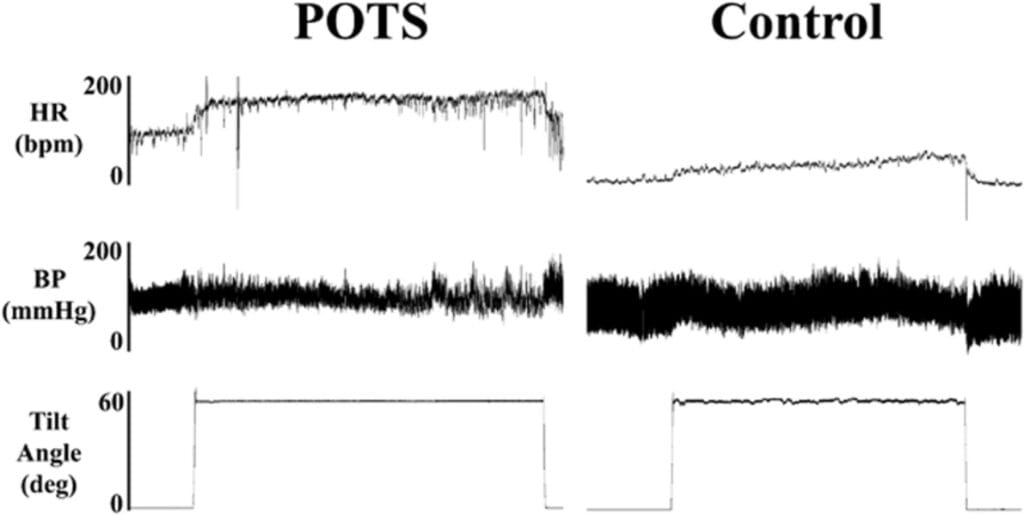
POTS is a disorder of the autonomic nervous system characterized by an excessive heart rate increase (≥30 bpm in adults, ≥40 bpm in adolescents) upon standing. This can lead to dizziness, fatigue, brain fog, palpitations, and, in some cases, fainting (syncope). It is commonly associated with conditions such as Ehlers-Danlos syndrome, chronic fatigue syndrome, and long COVID.
Symptoms of POTS
✔ Cardiovascular: Rapid heart rate, palpitations, dizziness, syncope (fainting)
✔ Neurological: Brain fog, headaches, difficulty concentrating
✔ Gastrointestinal: Nausea, bloating, constipation
✔ Musculoskeletal: Fatigue, muscle weakness, exercise intolerance
✔ Autonomic Dysfunction: Temperature dysregulation, excessive or reduced sweating
Causes & Risk Factors
✔ Neuropathic POTS – Small fiber autonomic nerve dysfunction leading to poor blood vessel control
✔ Hyperadrenergic POTS – Overactive sympathetic nervous system causing excessive adrenaline release
✔ Hypovolemic POTS – Low blood volume contributing to orthostatic intolerance
✔ Secondary POTS – Linked to conditions like Ehlers-Danlos syndrome, autoimmune diseases, or viral infections (e.g., COVID-19)
Underlying Mechanism of Fainting (Syncope) in POTS
Syncope in POTS is due to a combination of autonomic dysfunction, blood pooling, and inadequate cerebral perfusion when standing. Unlike vasovagal syncope, where blood pressure drops significantly, POTS-related syncope is primarily driven by an exaggerated heart rate response and abnormal blood flow regulation.
1. Orthostatic Stress (Standing Up) Triggers an Abnormal Response
- Normally, standing shifts 500-700 mL of blood to the lower body due to gravity.
- The autonomic system compensates with vasoconstriction and a mild HR increase (~10-15 bpm).
- POTS patients lack proper vasoconstriction, leading to excessive tachycardia (120-160 bpm) and blood pooling.
2. Blood Pooling & Reduced Venous Return
In neuropathic POTS, small fiber nerve dysfunction causes:
✔ Excessive blood pooling in the lower extremities
✔ Reduced venous return to the heart
✔ Lower stroke volume (amount of blood pumped per heartbeat)
📉 Result: Less blood reaches the brain, increasing syncope risk.
3. Compensatory Tachycardia & Sympathetic Overactivation
The body overcompensates by increasing heart rate excessively.
The sympathetic nervous system overreacts, releasing adrenaline and noradrenaline, causing:
✔ Further tachycardia (HR 120-160 bpm upon standing)
✔ Inefficient blood circulation
✔ Possible paradoxical blood pressure instability
📉 Result: Despite fast heart rate, blood is not effectively circulating to the brain.
4. Cerebral Hypoperfusion (Low Brain Blood Flow) & Syncope
- If the heart cannot compensate, blood pressure may drop, failing to maintain cerebral perfusion.
- Hyperventilation (from tachycardia) reduces CO₂, causing cerebral vasoconstriction and worsening brain oxygenation.
- The brain forces a “reset,” triggering syncope to restore blood flow when lying down.
5. Recovery Phase After Syncope
✔ Once the person falls or lies down, blood flow to the brain improves.
✔ Consciousness usually returns quickly (within seconds to minutes).
✔ Some patients experience post-syncopal exhaustion due to autonomic stress.
Factors That Worsen Fainting in POTS
✔ Prolonged Standing – Sustains blood pooling in the legs
✔ Heat Exposure – Causes vasodilation, worsening blood flow issues
✔ Dehydration or Low Salt Intake – Reduces blood volume
✔ Large Meals – Blood is diverted to the gut, reducing brain perfusion
✔ Exercise Intolerance – Exaggerated blood pooling and tachycardia post-exercise
✔ Hyperadrenergic Episodes – Sudden surges of norepinephrine destabilize BP
Diagnosis of POTS
✔ Active Stand Test or Tilt Table Test – Measures HR and BP changes upon standing
✔ Blood Tests – Assess hydration status, electrolytes, and autoimmune markers
✔ Autonomic Function Testing – Evaluates nervous system response
Treatment & Management of POTS
1. Lifestyle Modifications
✔ Increased Salt & Fluid Intake – Expands blood volume (2-3L fluids, 3-10g salt daily)
✔ Compression Garments – Reduces blood pooling (20-30 mmHg knee-high or thigh-high)
✔ Gradual, Structured Exercise – Reclined exercises like swimming and recumbent cycling
✔ Dietary Adjustments – Small, frequent meals to prevent postprandial hypotension
✔ Avoiding Triggers – Heat, alcohol, prolonged standing
Additional Lifestyle Strategies:
✔ Head Elevated Sleeping – Raising the head of the bed by 6-10 inches helps reduce morning dizziness.
✔ Leg Muscle Activation – Engaging calf muscles while standing improves circulation.
✔ Postural Adjustments – Moving slowly from sitting to standing prevents dizziness.
2. Medications for POTS
Fludrocortisone (Florinef) – Blood Volume Expansion
✔ Best for: Hypovolemic POTS
✔ Mechanism: Increases sodium and water retention
✔ Dosage: 0.05-0.2 mg once daily
Midodrine (ProAmatine) – Blood Vessel Constriction
✔ Best for: Neuropathic POTS
✔ Mechanism: Alpha-1 agonist that constricts blood vessels, preventing blood pooling
✔ Dosage: 2.5-10 mg three times daily
Beta-Blockers (Propranolol, Bisoprolol, Metoprolol) – Heart Rate Control
✔ Best for: Hyperadrenergic POTS
✔ Dosage:
- Propranolol: 10-60 mg/day
- Bisoprolol: 1.25-5 mg/day
- Metoprolol: 12.5-100 mg/day
Other Medications:
✔ Ivabradine – Selectively lowers HR without reducing BP
✔ Pyridostigmine – Enhances autonomic function for neuropathic POTS
✔ Clonidine or Methyldopa – Reduces adrenaline surges in hyperadrenergic POTS
Key Differences Between POTS Syncope & Vasovagal Syncope
| Feature | POTS Syncope | Vasovagal Syncope |
|---|---|---|
| Trigger | Standing up, prolonged standing, dehydration | Emotional stress, pain, sight of blood |
| Heart Rate Before Syncope | Rapid (120-160 bpm) | Initially increases, then slows |
| Blood Pressure Before Syncope | May be normal or slightly low | Drops significantly |
| Sympathetic Activity | Overactive (high adrenaline) | Parasympathetic dominance (vagus nerve overstimulation) |
| Recovery | Quick recovery but may feel exhausted | Quick but may feel weak after |
Key Takeaways for POTS Management
✔ Fludrocortisone – Expands blood volume (best for hypovolemic POTS)
✔ Midodrine – Prevents blood pooling (best for neuropathic POTS)
✔ Beta-blockers – Lowers heart rate (best for hyperadrenergic POTS)
✔ Lifestyle Adjustments – Essential for symptom control